What Causes Varicose Veins?
What Causes Varicose Veins and Spider Veins?
What Causes Varicose Veins? Risk Factors, Prevention and Treatment:
Varicose veins and spider veins are both caused by an underlying disease called venous insufficiency. Varicose veins are bulky, blue, twisted unhealthy veins that are often visible bulging from the skin surface. Small one-way doors called valves are scattered along the veins in the legs, preventing blood from falling back down towards the feet. Over time, these valves can become dysfunctional and blood leaks back past the valve, a condition known as venous reflux. The pressure increases in the veins below the valve and new spider and varicose veins form on the surface of the skin. If you suffer from varicose veins, you probably want to know what causes valve dysfunction and vein disease. We review risk factors and vein disease prevention, then talk about how to diagnose venous insufficiency and the best treatment options for varicose veins.
Book a consulation to see a vein specialist:
Questions? Call Us +1 (855) 807-4939
By emailing or contacting us, you are accepting the inherent privacy limitations of online communication. For more information, please read our Digital Communications document. Please respond “STOP” to any text messages to opt out.
What are causes and risk factors for varicose veins?
- Genetics: A family history of vein disease, spider veins and varicose veins makes it much more likely that you will develop this condition. If your mother and father both have vein disease, there is a 90% chance you will develop vein disease yourself.
- Female Gender: Men and Women are both at risk of developing varicose veins, but women are almost twice as likely to be diagnosed with vein disease.
- Age: Vein disease is uncommon before the age of 30, and your risk increases over time
- Pregnancy: Due to high circulating hormone levels, varicose veins and spider veins may increase over time.
- Weight Gain: Excess pounds put pressure on veins and makes it more likely you will develop spider veins.
What are varicose veins?
Varicose veins are large, unhealthy blue veins that are visible on the surface of the skin. Varicose veins tend to follow a tortuous, or twisted, path. They often bulge from below the surface of the skin, causing significant discomfort. They rarely appear before the age of 25, and they become more numerous with age.
Another type of unhealthy vein (also caused by venous insufficiency) is spider veins, or telangiactasias. Spider veins are smaller than varicose veins and tend to form in clusters that spread outwards on the surface of the skin. They may be red or purple in color.

What actually causes varicose veins? Venous Insufficiency explained:
Again, Varicose veins are caused by an underlying disease called venous insufficiency, which is a medical condition that affects the veins slightly deeper within the leg. All veins throughout the body have one simple task: to carry blood back to the heart after the oxygen in the blood has been used up by the body. This is more difficult for the veins in the legs than veins elsewhere because tgravity is constantly pushing the blood back down towards the feet. The leg veins work against gravity using something called valves. Valves are one-way doors that are scattered along the length of each leg vein. Blood flows up past a valve and the valve shuts, preventing the blood from falling back down to the feet.
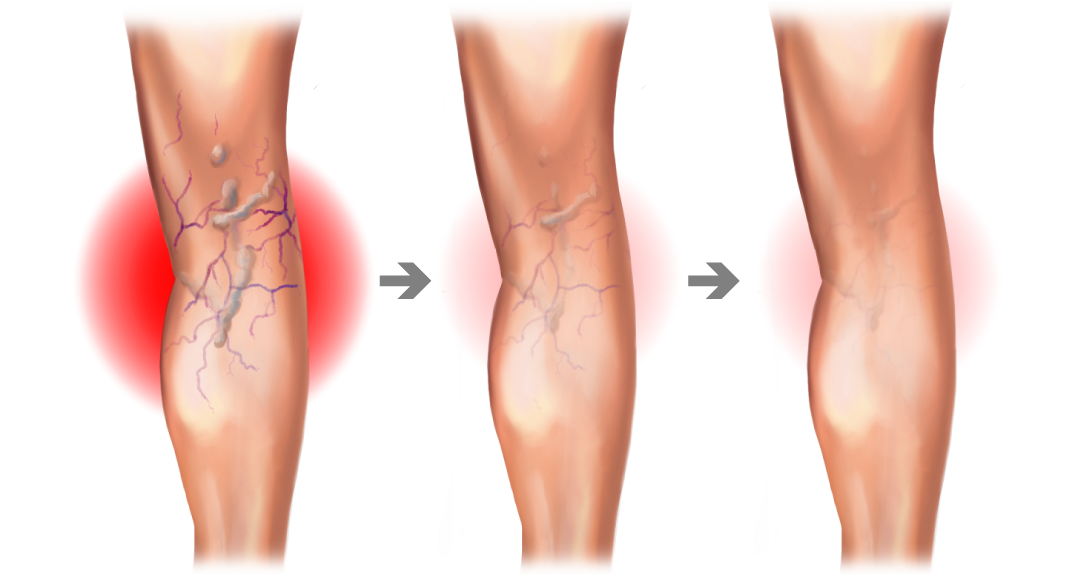
Over time, however, valves work less efficiently. Instead of stopping all the blood from falling down, they become leaky. Blood drops back down in the wrong direction. Below the valve, the vein is full of excess blood and may swell and bulge. The increased pressure leads to the development of new spider and varicose veins on the surface of the skin. The things that lead to valve dysfunction are exactly what causes varicose veins to form: genetics or a family history, weight gain, female gender, a history of Deep Venous thrombosis, also known as DVT or blood clots in the legs (the clots press up against the valves and damage them), and pregnancy.
How to Prevent Varicose Veins:
Some of the things that cause vein disease and varicose veins are non-modifiable, meaning you cannot avoid them. You cannot change your genetic makeup and you cannot change your biological gender. You can, however, do the following:
1. Maintain a healthy weight: Excess pounds put pressure on valves in the underlying veins
2. Exercise regularly: Exercising squeezes the muscles in the calf, which helps push blood up to the heart even if the valves aren’t functioning as well.
3. Avoid high heels: There is no firm evidence that wearing high heels or crossing your legs causes varicose veins, but both may lead to compression on the veins and decreased activity of the calf muscles, theoretically causing varicose veins.
4. Avoid prolonged sitting or standing: inactivity can lead to decreased circulation and more blood pooling in the legs. Try to walk at least a few minutes every hour.
5. Consider an evaluation for Venous Insufficiency: Monitor yourself for symptoms of vein disease. If you have underlying venous insufficiency, it’s more likely that your varicose veins will get worse.

How do you treat Varicose Veins?
Typically, treatment for varicose veins falls into two categories: Conservative (home remedies) and Procedures:
Conservative Treatments for Varicose Veins (Home Remedies):
Weight Loss
Obesity is a risk factor for varicose veins, and most doctors will encourage patients to pursue at least a trial of weight loss prior to attempting therapy.
Exercise
Even without weight loss, regular cardiovascular exercise can help improve circulation and improve symptoms of venous insufficiency and varicose veins. Pumping the calf muscle pushes blood up towards the heart.
Compression Stockings
Even without weight loss, regular cardiovascular exercise can help improve circulation and improve symptoms of venous insufficiency and varicose veins. Pumping the calf muscle pushes blood up towards the heart.
Essential Oils
There is some evidence that horse chestnut seed oil (Aesculus hippocastanum) may reduce symptoms due to varicose veins. Sea pine extract (Pinus maritima) may reduce edema (swelling due to vein disease). Other studies, however, question the efficacy of these medications.
Medical Treatments for Varicose Veins:
Sclerotherapy
In sclerotherapy, a medication called a sclerosant is injected into the vein. The sclerosant irritates the walls of the vein and causes an inflammatory response. Over time, the vein seals closed and is ultimately reabsorbed by the body. For larger veins, your doctor may mix the sclerosant with air, creating a foam, which allows vein doctors to fill a vein using less medication.
Radiofrequency Ablation (ClosureFast)
In radiofrequency, your doctor enters the vein with a thin device called a cathether. The catheter is positioned under ultrasound guidance along the length of the vein. Your vein doctor will surround the vein with a cooling, numbing fluid, then deliver heat (created by a radiofrequency generator attached to the catheter) to the walls of the vein. This causes the vein to seal closed and, over time, be reabsorbed by the body. Your doctor will perform this procedure under local anesthetic so you won’t any discomfort.
Laser Ablation
Laser ablation is very similar to radiofrequency ablation except the the heat source is a laser instead of a radiofrequency generator. Laser ablation is equally affective but slightly more uncomfortable compared to radiofrequency ablation.
Vein Glue (VenaSeal)
Vein Glue is the newest technology on the market for treatment of venous disease. A medical implant is carefully injected into the vein under ultrasound guidance, filling the vein and blocking blood flow.
Varithena
Varithena is a pre-made sclerosant foam (or premade foam sclerotherapy). Varithena is injected under ultrasound guidance, filling the varicose vein. Like traditional sclerotherapy, varithena causes an inflammatory reaction which leads to vein closure.
Phlebectomy
Phlebectomy, or surgical removal of the vein, is very rarely necessary due to the advent of the minimally-invasive technologies described above. On some occasions, however, your vein doctor may remove very small segments of a vein to disrupt flow, allowing other therapies to work more effectively.
What are Complications caused by Varicose Veins?
If left untreated, varicose veins may cause the following:
Bleeding: If a vein is under too much pressure, it may occasionally tear or burst, leading to bleeding.
Ulcers: poor circulation can lead to non-healing (or poorly-healing) wounds in the lower leg.
Stasis Changes: Impaired blood flow can lead to excess fluid retention in the lower legs, blood cells release a chemical called hemosiderin, which stains the skin a rusty-reddish color.
Who is the best doctor to treat varicose veins and venous insufficiency (the underlying cause of varicose veins)?
A qualified vein physician can come from several different medical fields, including vascular surgery, cardiothoracic surgery, anesthesiology, cardiology, internal medicine or even emergency medicine. Good vein physicians have excellent ultrasound skills and significant experience treating veins. Perhaps more important, an excellent vein physician will really listen to your concerns and find a solution that is customized for you. Veins are unique and vary from person to person, so the best treatment option may vary.