More than half of the American population suffers from some form of vein disease. If you are concerned that you might be one of them, you would want to learn a great deal about this significant healthcare problem. Our expert vein specialists from VTC answer your top questions about vein disease.
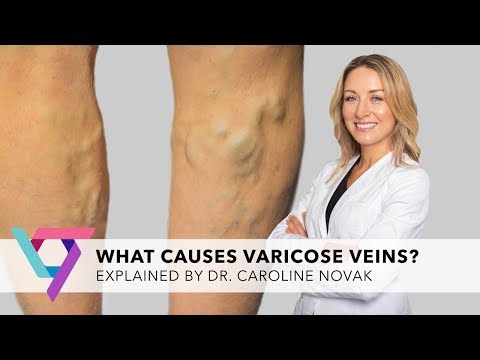
What are varicose veins and spider veins?
Varicose veins and spider veins are the commonest signs of vein disease. Varicose veins refer to the bulging, swollen veins that occur in the legs. These veins have a twisted appearance, and lie close to the surface of the skin. On the other hand, spider veins are smaller twisted blood vessels. Although they are visible, they do not bulge out. They can be bluish, reddish or purplish in appearance, and while they are most common in the legs, they can also occur in the arms and face. While varicose veins can run down the length of your leg, spider veins tend to occur in small clusters, with the inner part of your ankle being a common location.
Who is at risk of developing varicose and spider veins?
All older people, above 50 years can develop varicose or spider veins. They are more common in women, and pregnancy and menopause are independent risk factors for developing vein disease. The risk of developing these conditions increases if you are obese, smoke, or have a history of existing vein disease. Genetics is an extremely important risk factor, and if both your parents have varicose veins, there is a 90% chance that you will develop this condition as well.
What causes varicose and spider veins?
Varicose veins and spider veins are outward signs of an underlying vein disease, known as chronic venous insufficiency (CVS). This is a condition where the valves in your leg veins have become defective.

Your leg veins (mainly the saphenous vein) carry impure blood from the legs back to the heart. Since the blood has to travel a long distance, against gravity, there are tiny one-way valves at the top of the veins that assist with the process. Once the blood flows past, the valves close and prevent the blood from falling back into the leg.
If these valves become defective, blood begins to accumulate in the leg veins. This causes the vein walls to expand under pressure, and the vein bulges outward. Smaller branches from the vein can also get affected by the increased pressure, and this leads to the formation of new varicose and spider veins.
Should I get treated for varicose and spider veins?
In one word – yes. If left untreated, varicose and spider veins can eventually cause painful symptoms that decrease your quality of life. These include heavy, aching legs, swelling of the ankles and feet, and general fatigue. The area near the defective veins may become discolored and itchy. Over time, you can also develop cramps or throbbing pain in your legs.
Long standing vein disease can also have more serious complications. The blood circulation in your legs is compromised, so wounds may not heal effectively. Even minor scratches or scrapes can turn into open wounds and non-healing venous ulcers. If the bulging varicose vein gets injured directly, you can have profuse bleeding that may be difficult to control. One of the most dangerous complications, however, is deep vein thrombosis, which is the formation of blood clots within the veins. If these clots travel though the heart to the lung, they can block the blood vessel to the lung and can potentially be fatal.
What are the treatment options for varicose and spider veins?
There are several treatment options available. Ideally, you need to stop blood from flowing through the defective vein. This was earlier accomplished by removing the entire vein, an invasive surgical procedure called vein stripping. Nowadays, there are minimally invasive treatment options that simply seal off the vein so that blood can no longer flow through it. Over time, the defunct vein gets absorbed by the body, and blood flows through healthier veins.
These minimally invasive procedures include:
- Radiofrequency Ablation: The skin over the vein is numbed, and incised. A radiofrequency catheter is inserted into the vein. When activated, the heat seals the vein.
- Endovenous Laser Ablation: A laser fiber is used instead of a radiofrequency catheter.
- Venaseal: Medical grade glue injected into your vein seals it off.
- Sclerotherapy: Injection of medicated solution directly into the defective vein to scar it and seal it. This is used for small spider veins.
- Varithena: Medicated foam is injected into your veins. This covers more area than a sclerosant, and can be used for medium veins
- Clarivein: A tiny device is implanted into your vein, which disperses sclerosant throughout the vein.
Is it safe to get minimally invasive treatment for varicose and spider veins?
Absolutely! The adverse effects of minimally invasive treatment are very, very rare. There is a slight possibility of developing an allergic reaction to the medicated solution used. Very rarely, you may develop an infection or a blood clot at the procedure site.
Bear in mind that the chances of adverse effects (especially infections and clots) are even less when you see an experienced vein doctor. Choose a reputed vein clinic, and a board-certified, trained vein specialist who is skilled at performing minimally invasive treatment for vein disease.
If you have more questions about vein disease, our experts at Vein Treatment Clinic are happy to help! Book an appointment at any of our clinics online, or call (844) 690-1788 today!