At Vein Treatment Clinic, we understand the discomfort and frustration of varicose veins. These twisted, swollen veins not only mar the appearance of your legs but can also cause pain and other health issues if left untreated. Fortunately, several effective strategies for managing varicose veins can help you find relief and regain confidence in your legs. In this guide, we’ll explore the best varicose vein management strategies to help you make informed decisions about your vein health.
At Vein Treatment Clinic, we understand the discomfort and frustration of varicose veins. These twisted, swollen veins not only mar the appearance of your legs but can also cause pain and other health issues if left untreated. Fortunately, several effective strategies for managing varicose veins can help you find relief and regain confidence in your legs. In this guide, we’ll explore the best varicose vein management strategies to help you make informed decisions about your vein health.
1. Compression Therapy
Compression therapy is one of the most widely recommended strategies for managing varicose veins. By wearing compression stockings, you can improve blood flow in your legs and reduce swelling and discomfort associated with varicose veins. These specially designed stockings apply gentle pressure to your legs to support the veins and prevent blood from pooling. For optimal results, it’s essential to wear compression stockings consistently and choose the right level of compression based on your needs.
Benefits of Compression Stockings:
- Improved Blood Circulation: Compression stockings help enhance blood flow in your legs, reducing the risk of blood pooling and clot formation.
- Reduced Swelling: The gentle pressure applied by compression stockings helps minimize swelling and discomfort associated with varicose veins.
- Pain Relief: Compression stockings can alleviate pain and achiness caused by varicose veins by providing support to the veins and surrounding tissues.
- Prevention of Complications: By promoting healthy blood flow and reducing swelling, compression stockings can help prevent complications such as skin ulcers and blood clots.
- Enhanced Comfort: Wearing compression stockings can make standing and walking more comfortable, allowing you to go about your daily activities with greater ease.
- Convenience: Compression stockings are easy to incorporate into your daily routine and can be worn under clothing without anyone noticing.
- Long-Term Management: Regular use of compression stockings can help maintain the results of other varicose vein treatments and prevent the recurrence of varicose veins.
2. Lifestyle Changes
Making simple lifestyle changes can significantly impact varicose veins. Regular exercise, such as walking or swimming, can improve circulation and strengthen the muscles that support your veins. Additionally, maintaining a healthy weight can reduce pressure on your veins and decrease the risk of developing new varicose veins. Elevating your legs when resting and avoiding long periods of standing or sitting can also help alleviate symptoms.
Lifestyle Changes to Improve Vascular Health:
- Regular Exercise: Engage in low-impact exercises like walking, swimming, or cycling to promote circulation and strengthen leg muscles.
- Maintain a Healthy Weight: Excess weight puts added pressure on your veins, so strive to maintain a healthy weight through a balanced diet and regular exercise.
- Avoid Prolonged Sitting or Standing: Take breaks to stretch and move throughout the day, and avoid long periods of sitting or standing to prevent blood from pooling in your legs.
- Elevate Your Legs: When resting, elevate your legs above heart level to reduce swelling and improve blood flow back to the heart.
- Stay Hydrated: Drink plenty of water throughout the day to keep your blood flowing smoothly and prevent dehydration, which can exacerbate vein issues.
- Wear Comfortable Shoes: Choose supportive, low-heeled shoes that promote good posture and circulation, avoiding high heels or tight-fitting shoes that restrict blood flow.
- Quit Smoking: Smoking damages blood vessels and impairs circulation, so quitting smoking can significantly improve vascular health and reduce the risk of varicose veins.
- Eat a Balanced Diet: Consume a diet rich in fiber, fruits, vegetables, and lean proteins to support vein health and prevent constipation, which can contribute to varicose veins.
3. Dietary Adjustments
What you eat can play a crucial role in managing varicose veins. A diet rich in fiber can prevent constipation, which can contribute to varicose veins by increasing pressure on the veins in your lower body. Foods high in antioxidants, such as fruits and vegetables, can help protect your veins from damage caused by free radicals. Additionally, incorporating foods that are high in vitamin C and flavonoids can promote vein health and strengthen vein walls.
Dietary Tips to Support Vein Health:
- High-Fiber Foods: Incorporate foods rich in fiber, such as whole grains, legumes, fruits, and vegetables, to promote healthy digestion and prevent constipation.
- Hydration: Drink plenty of water throughout the day to maintain proper hydration levels and support optimal blood flow and circulation.
- Omega-3 Fatty Acids: Include sources of omega-3 fatty acids, such as fatty fish (salmon, mackerel, sardines), flaxseeds, and walnuts, in your diet to help reduce inflammation.
- Antioxidant-Rich Foods: Consume foods high in antioxidants, such as berries, citrus fruits, leafy greens, and nuts, to protect your veins from oxidative stress and damage.
- Vitamin C: Incorporate foods rich in vitamin C, such as oranges, strawberries, kiwi, and bell peppers, into your diet to support collagen production and strengthen vein walls.
- Flavonoid-Rich Foods: Include foods high in flavonoids, such as onions, garlic, citrus fruits, and dark chocolate, to help improve vein function and reduce the risk of varicose veins.
- Moderate Salt Intake: Limit your intake of salty and processed foods, as excess sodium can contribute to water retention and swelling, exacerbating symptoms of varicose veins.
- Limit Alcohol Consumption: Excessive alcohol consumption can dilate blood vessels and impair circulation, so drink alcohol in moderation to support vein health.
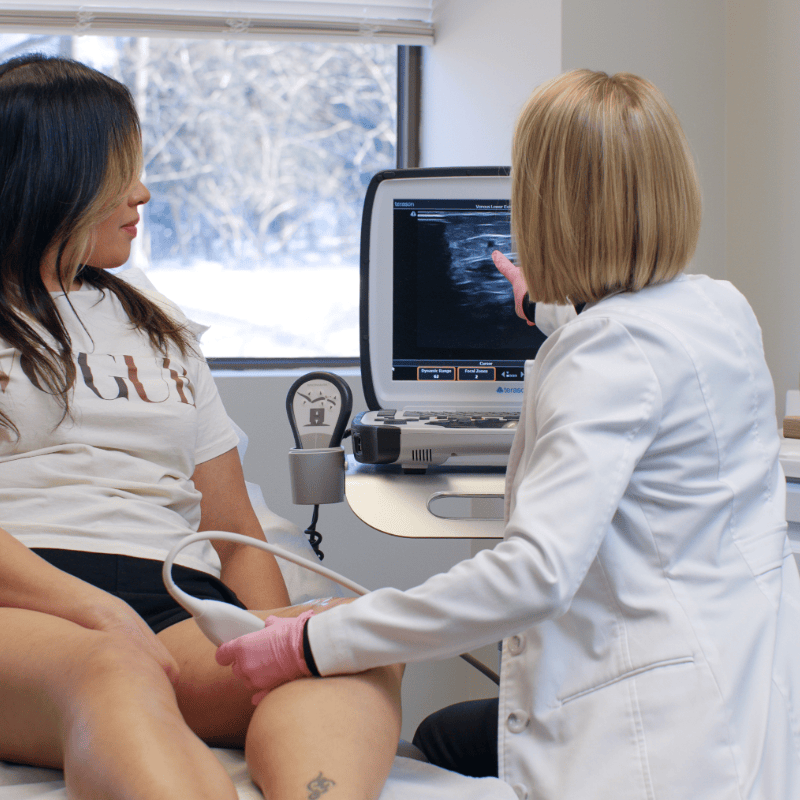
4. Minimally Invasive Treatments
Lifestyle changes and conservative treatments can alleviate symptoms, but they can’t remove varicose veins or treat the root cause. That’s where minimally invasive treatments come in. Procedures such as endovenous laser therapy (EVLT) and sclerotherapy can effectively treat varicose veins by closing off the affected veins or causing them to collapse and fade away. These treatments are performed in-office and require minimal downtime, allowing you to resume your daily activities shortly after treatment.
Your Minimally Invasive Vein Treatment Options:
- Endovenous Laser Ablation: A minimally invasive procedure that uses laser energy to seal off varicose veins. The laser heats the vein from the inside, causing it to collapse and be reabsorbed by the body.
- Radiofrequency Ablation: Similar to endovenous laser ablation, radiofrequency energy is used to heat and close off the affected vein. The heat from the radiofrequency energy causes the vein to collapse and eventually be absorbed by surrounding tissues.
- VenaSeal: A newer minimally invasive treatment that uses a medical adhesive to seal varicose veins shut. A small amount of medical adhesive is injected into the affected vein, sealing it off and rerouting blood flow to healthier veins. VenaSeal requires no anesthesia and has a quick recovery time, allowing patients to resume normal activities immediately.
- ClariVein: A procedure that combines mechanical and chemical ablation techniques to treat varicose veins. A rotating catheter is inserted into the vein, where it delivers a sclerosing agent to irritate the vein walls and seal them shut. ClariVein is often performed under local anesthesia and offers minimal discomfort and downtime.
- Ambulatory Phlebectomy: A surgical procedure used to remove large surface varicose veins through tiny incisions in the skin. Ambulatory phlebectomy is typically performed on an outpatient basis under local anesthesia. This procedure can be an effective option for removing visible varicose veins and improving the cosmetic appearance of the legs.
- Sclerotherapy: A minimally invasive treatment that involves injecting a sclerosing solution directly into varicose veins. The solution irritates the vein walls, causing them to collapse and eventually be reabsorbed by the body. Sclerotherapy is often used to treat smaller varicose veins and spider veins and can be performed in the office with little to no downtime.
5. Regular Monitoring and Follow-Up
Managing varicose veins is an ongoing process that requires regular monitoring and follow-up care. Even after successful treatment, it’s important to continue practicing healthy habits and keeping an eye out for any new or recurring symptoms. Our team at Vein Treatment Clinic is dedicated to providing comprehensive care and support to help you maintain optimal vein health long-term. We’ll work with you to develop a personalized treatment plan and schedule regular check-ups to ensure that your varicose veins remain under control.
Manage Varicose Veins & Maintain Optimal Vein Health
Varicose veins may be a common concern, but they don’t have to dictate your quality of life. With the right management strategies, you can find relief from discomfort and regain confidence in your legs. From compression therapy and lifestyle changes to minimally invasive vein treatments, there are plenty of options to help you take control of your vein health. At Vein Treatment Clinic, we’re here to support you every step of the way on your journey to healthier legs — schedule an appointment with our board-certified vein doctors in New York, New Jersey, California, or Maryland.